“Decisions you have never made before”
Medical Improvisations in a COVID ICU
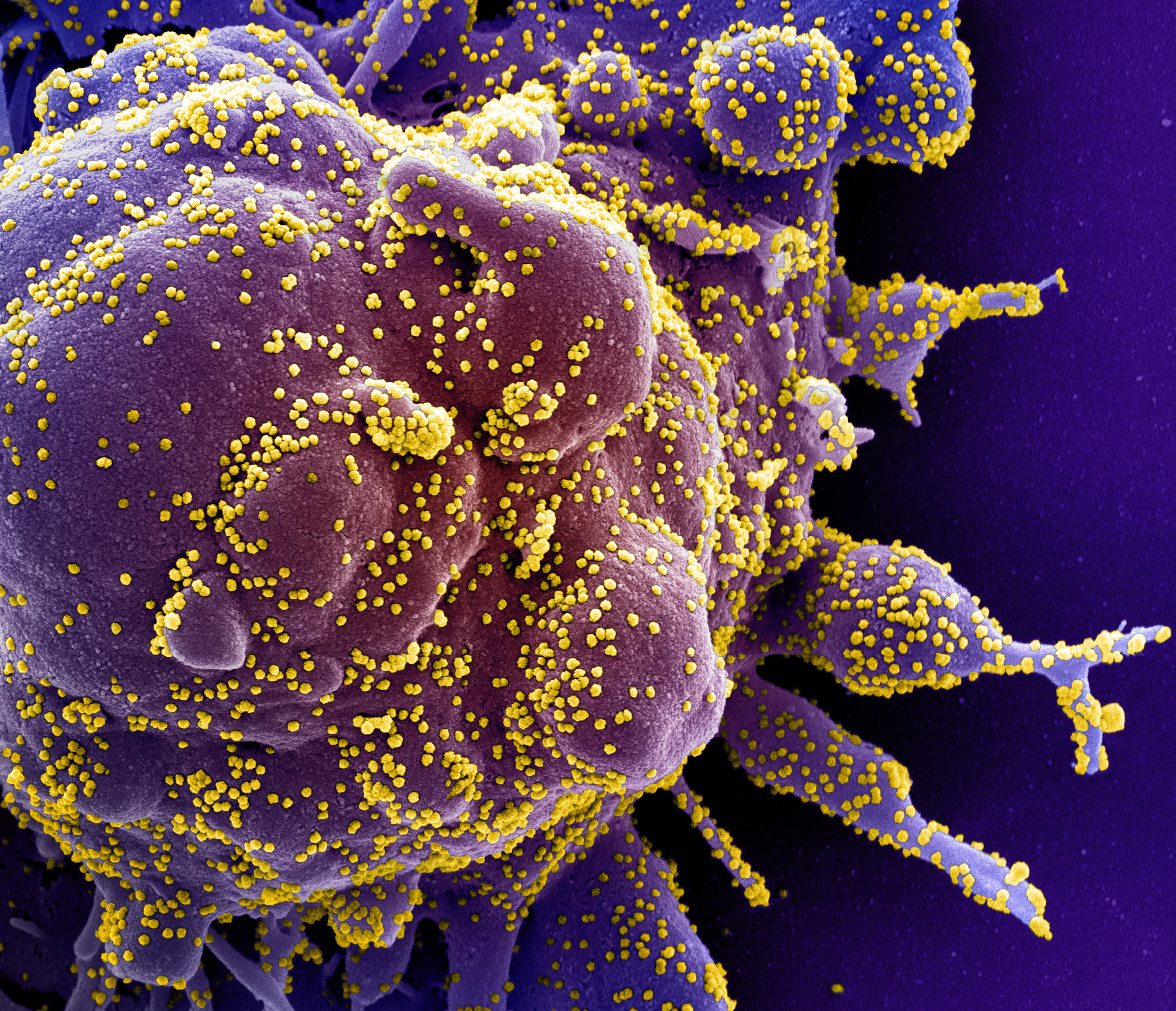
Source: NIAID-RML/ Flickr CC.BY.2.0
This article is part of our “Reflecting on COVID-19” series.
If you’d like to check out other articles in this series, click here.
The author is a practicing surgeon who volunteered early in the pandemic to staff an expansion intensive care unit at a hospital in the northeast United States. The following reflections are adapted from a record, or journal, that was prepared during a rare break at the request of the author’s family, who asked to know what was going on during the crisis. It has been lightly edited for this format and is shared in hopes that it may be useful to others.
In anticipation of running a makeshift ICU, as my hospital expands capacity, I am watching videos on ventilator management and reading all 300+ pages of a Department of Defense publication on the management of COVID. I rounded in the regular surgical ICU, just to get a sense of what everyone here is doing. There is a tremendous political divide between medicine and surgical teams, and we have been as unsuccessful achieving bipartisan efforts in our hospital as we have in politics.
Tonight I move into a hotel. Thinking about it as a deployment is helping, mentally. Meanwhile one of my colleagues is critically ill with the virus, while another is on the mend.
In the five or so minutes I tried to engage on social media, I posted something mildly suggestive of our impending hospital shortages. It was picked up by my institution, and I was asked to delete it, as it was not quite “on message.” I also saw a post by someone that I regret not capturing. It said, and I paraphrase: In the next few weeks you will be asked to make decisions you have never made before, and never thought possible. You are absolved. You will be asked to do things you were not trained for. You are absolved. People will die under your care, alone. You are absolved.
First impressions of an unknown enemy
We have realized in the last 24 hours that COVID-19 is a clotting disease. Starting immediately I am thinning the blood of all patients under my charge. I (and others) suspect there may be some platelet stickiness effect; therefore I’m also going to start patients on simple aspirin. I have no clue as to whether I’m barking up the wrong tree, but we’re starting a non-blinded, non-randomized trial in the hospital with expedited approval. I don’t think the clotting nature of the blood is related to transmission, however, once the disease sets in, it may be related to severity of the disease.
I meant to write all of this down on [–––] but I started my four-day ICU shift that evening. We rotate. We don’t come up for air until the four days are over. I take a 9 p.m. phone call the night before I’m scheduled to take over with a person in the ICU to tuck people in before they go to bed. That afternoon, we’d gotten several admissions just before we left, which would exemplify one way that this disease can go.

If you’ve been reading about this disease at all, you know the way that it kills people is that it sets off an inflammatory reaction that is native to the body, but that is so profound in its strength that it overwhelms all organ systems. In most areas of medicine, if someone is getting sick and you put them on a ventilator, with that crucial extra support the body is actually able to rest, even momentarily. The doctor rescues them, allows them to recover, and then removes the support (the ventilator) when it’s time. We intubate COVID patients when they are getting sicker, since intubation buys time for patient and doctor. However, we have also learned that the event of intubation pushes many individuals over the edge into what has been termed a “cytokine storm.” In the 24 hours following intubation every single body system tries to shut down, and we then do everything in our power to try and stop each and every one from doing that.
In the 24 hours following intubation every single body system tries to shut down, and we then do everything in our power to try and stop each and every one from doing that.
The blood pressure plummets. This happens so fast that when we hear of a patient coming down to our unit we order blood pressure medications on some random patient, because if we wait to order them for our future patient, he’ll be dead before they come over from pharmacy. This timeline is somewhat unique to my position in a makeshift ICU, but is also secondary to the highly compressed COVID disease timeline, in comparison to even the most severe illness that we’ve dealt with before now, before this phenomenon. The low blood pressure can be a shock not only to the heart but also to the liver. Some people with perfectly normal hearts have suffered heart failure.
After the intubation a patient’s lungs get increasingly hard to ventilate, requiring maximum concentrations of oxygen and maximum pressures. We have to force the oxygen into the lungs, even though half an hour ago this very patient was breathing on their own. Sometimes it’s so difficult to ventilate the lung that we are forced to paralyze the patient, to ensure that no spontaneous muscle movement interferes with the work of the ventilator. We immediately flip the patients on their stomachs, as “proning” helps open up areas of the base of the lung that get compressed when lying flat. Sometimes proning is the only thing that will save a patient’s life, but the act of flipping them over can be so traumatic so as to cause cardiac arrest. More than once I’ve told the proning team of nurses, who are my friends, that they may be saving the life of the patient they are about to turn … but that this man’s heart may stop in the process.
If so, it’s not their fault. It’s not their doing.
The kidneys shut down. I usually need to give patients 2-3 liters of fluid in the first 24 hours in order to keep the kidneys from failing. COVID plus kidney failure equals more than 95% mortality. Convention states that with Acute Respiratory Distress Syndrome you need to keep patients relatively “dry,” but we thought that was leading to kidney failure. So we tried giving fluid and it worked.

I have not had to put a single patient on dialysis that has come to my unit, and around the hospital the word about fluid is spreading.
I have learned that for some patients, no matter what I do, within 24 hours they are dead. This has happened a handful of times, and it is incredibly traumatic. It happened the evening of [–––] during the 9 p.m. phone call, and the following morning, and the following afternoon. Three patients showed up in my unit that day and despite an incredible force of support on our part, died—spectacularly—within four, sixteen, eighteen hours. This was a bad day.
If we get patients to make it through the first 24 hours, then the next 4-5 days are tentative at best. We throw just about every medication we have at them. Antibodies against immune mediators to slow the flood of immune cytokines that we think leads to death. Blood pressure medications to raise the blood pressure. Antibiotics, though the prevalence of bacterial coinfection is low. Steroids. Full-dose blood thinners, as we know this disease causes clot. We get about 20 labs a day, and check them all, on a dozen patients in this M.A.S.H. unit. When patients are prone they can kink their breathing tubes, or else the disease causes such bad secretions into the lungs that the tube fills up and clogs. This leads to several harrowing moments every single day where, before my eyes, someone literally stops being able to breathe—though they are fully connected to a machine that is supposed to breathe for them—and then I’ve got 1-2 minutes to figure out and fix what’s wrong. At least twice a day someone’s pulse starts to race, or their blood pressure plummets inexplicably, and then I’ve got 1-5 minutes to fix that. Or their potassium shoots up to life-threateningly high, or their pH plummets to life-threateningly low. Both times I’ve got 1-5 minutes to push some medications that buy me maybe thirty minutes to track and figure out the source and then come up with a better, longer term solution. Every day between two and five people try to die in exactly these ways, and I can’t predict how or when or even which person. It feels like every day I’m defusing a bomb. Two to five bombs.
It feels like every day I’m defusing a bomb. Two to five bombs.
During these days our team’s conversations with a worried family are surreal, as there is no possible way that a family in this state of mind can understand just how sick their father or uncle or grandmother is, or how much medicine—both the physical and the intellectual—is going into keeping them alive. The most accurate thing I can say to them is: “He’s alive now, but I can’t tell about this afternoon, or tonight, or tomorrow.” My predictive algorithms and instincts, trained and honed through my career, simply don’t work here. The paradigms of disease and treatment, action and response, are completely flouted by this disease. It would be paralyzing, if you had time to think.
Assuming patients manage to make it through this, we have seen a few of them settle. The disease runs its course. Maybe on day seven or eight or nine we can start to take breathing tubes out of people. This phase is so important, and yet we were deprived of it at the start of everything. Due to overwhelming pressures on the hospital, all acute ICU units like this one were needed for the deluge, and the most severe of cases. As soon as I manage to help one patient to survive the acute phase, he or she was shipped off to another unit, or to another hospital, with more room, and immediately I got another fresh patient. The death rate was incredibly—understandably—high, in the pre-ICU period, particularly when the lessons we scrambled to learn, like the importance of fluids, had not yet translated into different care.
My predictive algorithms and instincts, trained and honed through my career, simply don’t work here. The paradigms of disease and treatment, action and response, are completely flouted by this disease.
I made every effort to witness the autopsy of the woman in my care who’d only managed to survive 18 hours after her intubation. We’d actually been able to keep her off the ventilator in our unit for five days prior to this, her decompensation. We’d thrown the book at her. All the medications, full dose anticoagulation, plenty of fluids. Despite this, her inferior vena cava, liver, and lungs had clots in them that were shaped like they’d come up from the legs. Less clot burden, I was told by the pathologist, than those patients not anticoagulated. Certainly more than should be there, given how much heparin (blood thinner) I gave this woman. Her kidneys demonstrated Acute Tubular Necrosis despite the fluids. It was evident in the labs we’d seen in the hours before her death, a death so quick that these fluids wouldn’t have had time to help. Her heart muscle was entirely, homogeneously diseased. Her labs suggested she was having a heart attack, but the dead muscle wasn’t in the distribution of the coronary artery. It was global. The pathologist was trying to find the virus in the muscle cells. An alternative hypothesis was this virus creates a toxin of some kind that causes damage to the heart cells.
I saw a clot that had formed within the heart. It had not traveled there, but settled in directly. The pathologist told me that what she’d seen, macroscopically and microscopically, was a host of wildly different problems combined. Hemolytic uremic syndrome (clotting, red blood cell destruction, and kidney damage), disseminated intravascular coagulation (where blood spontaneously clots within blood vessels), macrophage activating syndrome with hemophagocytic lymphohistiocytosis (one type of immune cell ingests red blood cells), and diffuse alveolar damage (a disease process in the lung) all together. HUS, DIC, MAS with HLH, DAD … these labels we’d put on phenomena that were mere subsets of the havoc wreaked by this pathogen. It made me think that our desperate strategy to throw the kitchen sink at patients, which for a time seemed a bit indiscriminate and simple-minded, might indeed be the right response.
While we don’t yet have a magic bullet, I can say with confidence that we are smarter about how we do things. Since last week each new admission from the floor has survived.
Even as I record this I’m not sure I want anyone to read it. Anyone who knows someone who has COVID. What I see every day are the worst of the worst cases, and my impression is biased. Statistically speaking, someone in my circle of friends and family will get it, someone in your circle of friends or family will get it, and even though statistically speaking, that person will be fine, the person who reads these things will become terrified for them. If I cause that pain for you, whoever you are, I’m sorry. I’ve also been able to rescue people from the brink, and while we don’t yet have a magic bullet, I can say with confidence that we are smarter about how we do things. Since last week each new admission from the floor has survived. There are more and more donors of ‘convalescent plasma’—individuals who have been sick, and recovered, and hope to spare others the experience. What we don’t know is the right time or way to give the donated plasma (rich with what we hope are antibodies and other factors that will someday be catalogued and quantified). For now I know that hundreds of the things I’ve done will be determined to have been useless, and some will be determined to have been potentially harmful. And yet what is the alternative? We are making this up as we go along.
For the moment my shift is over. In a day or two I will plunge back in. As of tonight, one quarter of our entire hospital is intubated.
One last thing. I made sure to go and watch a presentation by the pathologist who performed that autopsy on my patient. She showed slides of the heart, the lung, and the kidney. Everything she said she’d already told me in the autopsy suite. Yet the summary of information seemed vital; there were 200 attendees on the phone. Surgeons, intensivists, oncologists, administrators, rheumatologists, infectious disease specialists, nephrologists, people who were taking care of the patients an hour ago, and would an hour later. Then she showed something I hadn’t seen: an electron micrograph of the virus, COVID-19, inside a cell. It was exactly as I would have drawn it if asked by my eight-year-old niece. It was like looking at—finally seeing—the face of a murderer. ♦
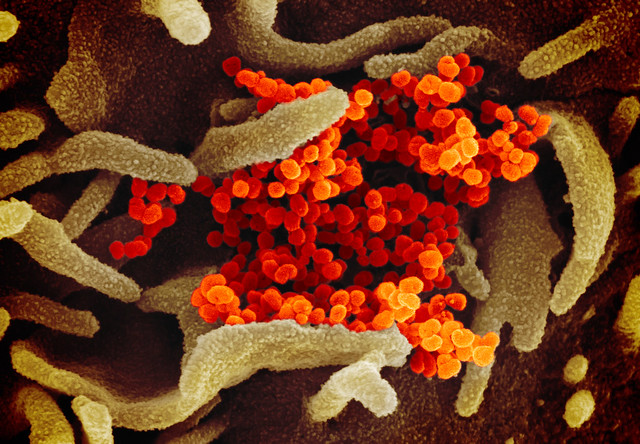
Source: NIAID’s Rocky Mountain Laboratories (RML) in Hamilton, Montana, produced images of the novel coronavirus (SARS-CoV-2, previously known as 2019-nCoV) on its scanning and transmission electron microscopes on Tuesday, Feb. 11, 2020. Read more [here].
In the midst of the global COVID-19 pandemic, Canopy Forum continues our commitment to produce expert analysis for the broader community of digital consumers: citizens, scholars, lawyers, clergy, journalists, policy makers, and more. We’ve collected our recent content reflecting on the current public health crisis here, as well as some of our latest articles below.
- Selling Religious Cures and Other First Amendment Pitfalls in the Age of Coronavirus by Shlomo C. Pill
- Defiant Congregations in a Pandemic: Public Safety Precedes Religious Rights by Tanner J. Bean, Brian A. Smith, and Robin Fretwell Wilson
- An Early Good Friday, at Last: When Too Many Bells Toll in Italy by Andrea Pin
- A Plague of Confusion: Coronavirus and Passover by David R. Blumenthal
Recommended Citation
“‘Decisions you have never made before’ – Medical Improvisations in a COVID ICU.” Canopy Forum, April 16, 2020. https://canopyforum.org/2020/04/16/decisions-you-have-never-made-before-medical-improvisations-in-a-covid-icu/

